Mask Myth Busters: What You Need to Know About Personal Protection

Wearing a mask to prevent the spread of Covid-19 has evolved into a fiercely debated topic lately, and an abundance of disinformation exists. At Hemp Black and our sister company, Ananda Health, we regularly address the confusion around the hemp and CBD space. We are no stranger to dispelling myths and have earned a reputation for providing honest, evidence-based answers. Here, we address the important questions surrounding masks or face coverings in the time of coronavirus.
Myth 1: Masks do not help stop the spread of Covid-19
Social distancing is not always possible. Even when it is, new data suggests 6 feet may not be enough. The Journal of the American Medical Association (JAMA) published a report that infectious respiratory droplets can travel up to 27 feet. Face coverings limit this mode of transmission, significantly decreasing overall spread of Covid-19. In fact, new research shows that that masks decrease transmission by 75%.
Compare New York City, now the epicenter of the outbreak with the highest number of cases worldwide, to Hong Kong. Hong Kong is even more densely populated than New York City, with similar widespread reliance on crowded public transportation. Moreover, Hong Kong has a direct connection via high-speed train to Wuhan, China, the origin of the outbreak. These risk factors mean Hong Kong was the ideal setting for an even larger outbreak than New York City. But that didn’t happen. As of early June 2020, Hong Kong has reported only 1,108 cases and 4 deaths due to Covid-19, whereas New York City has reported over 207,000 cases and 17,127 deaths. Experts agree that Hong Kong successfully contained the virus because of early and widespread use of masks and face coverings.
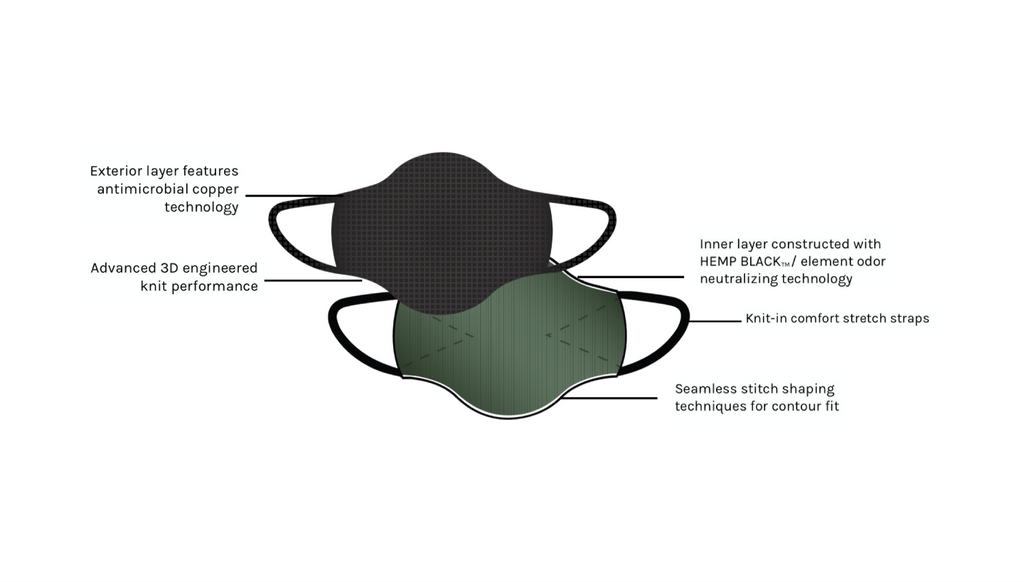
Masks and other face coverings, such as a neck gaiter, offer the wearer some limited protection of contracting Covid-19 because they act as a physical barrier between the environment, where viral particles exist, and the mucous membranes in the nose and mouth, where viral particles replicate and cause infection. Viral particles are so small, however, that they may penetrate some masks. Masks made with copper technology however, offer better protection as the virus can make contact with a material capable of killing SARS-CoV-2, the virus that causes Covid-19.
However, the primary motivation for wearing a mask is to reduce the chance of infecting other people. Those who feel perfectly healthy can unknowingly transmit the coronavirus. This is due to asymptomatic and presymptomatic infections. Asymptomatic infections refer to those who are infected with the coronavirus but who never experience any symptoms. They never have any indication that they are infected, but they are shedding the virus through talking, breathing, sneezing, etc., leaving viral particles in their wake for someone else to host. Multiple studies have shown that 25-80% of coronavirus cases are asymptomatic. In Iceland, public health researchers reported that 50% of cases were asymptomatic. Another study on a cruise ship identified that 104 out of 128 (81%) of positive cases were asymptomatic.
Presymptomatic means someone is in the early stages of infection, before symptoms appear. This is different from asymptomatic transmission in that presymptomatic patients eventually go on to develop symptoms, whereas asymptomatic patients never develop symptoms. In other viruses, and even similar viruses including another coronavirus that causes SARS, symptom onset often occurs simultaneously with viral shedding. That makes them easier to control. In these outbreaks, as soon as someone is infectious, they exhibit symptoms, which in turn alerts them to the need to self-isolate. With Covid-19, however, research presents a different case: Symptom onset does not occur simultaneously with infectiousness. A study from Singapore concluded that viral shedding occurs at least 1-3 days before symptoms occur and a follow-up study in the New England Journal of Medicine revealed that viable viral cultures were present in patients up to 6 days before symptom onset. Because the new coronavirus actively replicates in the upper respiratory tract, transmission can occur easily by just by breathing or talking. For comparison, mild or asymptomatic cases of the flu exhibit low viral count in the upper respiratory tract compared to the lower respiratory tract, which makes transmission more difficult. In lower respiratory tract viruses, transmission is more likely to occur with secretions from the lower respiratory system, such as coughing, and less likely to occur with upper respiratory secretions, such as talking. In fact, viral load of the new coronavirus is highest at or before symptom onset, and researchers concluded that 44% of cases were due to presymptomatic exposure. Those without symptoms, whether they go on to develop them or not, seem to be just as capable of infecting others as those with current symptoms. Research from Italy shows that viral load did not differ between symptomatic and asymptomatic cases of Covid-19.
One study however, contradicts some of this. Researchers in China identified 455 contacts of a positive but asymptomatic Covid-19 carrier. None of the contacts exhibited symptoms, and they all tested negative for Covid-19 on nucleic acid tests. This sample suggests that transmission risk may be low in asymptomatic carriers, but the results need to be considered along with multiple conflicting studies noted above. Additionally, the nucleic acid test used in this study is not always accurate and can produce false negatives. Until and unless this data is replicated, err on the side of caution and take it with a grain of salt.
On June 8th 2020, the World Health Organization (WHO) issued reassuring opinion that new data suggests asymptomatic transmission of Covid-19 is rare, but the CDC has not weighed in yet. Dr. Ashish Jha, Director of the Harvard Global Health Institute maintains that infected people without symptoms are an important cause of spread. Nonetheless, remember that asymptomatic cases differ from presymptomatic cases, and presymptomatic patients shed the virus and risk infecting others for days before developing symptoms. Additionally, many cases of Covid-19 are mild and may be confused with something as benign as seasonal allergies. Other cases may present atypically, with symptoms including digestive upset, rash, or even “Covid toe.” These presymptomatic, mild, and atypical cases are distinct from asymptomatic cases and contribute to increased contagion. Prolonged isolation for everyone would solve this issue, but that is an impossible solution. A barrier in the form of a face covering, however, is the next best defense.
 Now that we’ve covered the relative risks of presymptomatic and asymptomatic transmission, that bring us to whether or not masks actually do anything to prevent infections. Scientific evidence overwhelmingly supports that masks reduce infection rates. A 2008 study evaluated respirators, surgical, and homemade cloth masks and concluded that “any type of mask is likely to decrease viral exposure and infection risk on a population level,” even with imperfect fit and adherence. A more recent analysis considered biology, mechanics, and “cough droplet ballistics” of the new coronavirus and a statement issued in late April from the esteemed Mayo Clinic makes a compelling, factual case for masks. Last, Jeremy Howard of the University of San Francisco published an article establishing the case for masks. His research institute identified 34 scientific papers to support that masks, including cloth masks, can reduce viral transmission, with zero evidence to the contrary.
Now that we’ve covered the relative risks of presymptomatic and asymptomatic transmission, that bring us to whether or not masks actually do anything to prevent infections. Scientific evidence overwhelmingly supports that masks reduce infection rates. A 2008 study evaluated respirators, surgical, and homemade cloth masks and concluded that “any type of mask is likely to decrease viral exposure and infection risk on a population level,” even with imperfect fit and adherence. A more recent analysis considered biology, mechanics, and “cough droplet ballistics” of the new coronavirus and a statement issued in late April from the esteemed Mayo Clinic makes a compelling, factual case for masks. Last, Jeremy Howard of the University of San Francisco published an article establishing the case for masks. His research institute identified 34 scientific papers to support that masks, including cloth masks, can reduce viral transmission, with zero evidence to the contrary.
The aforementioned sources consider the physics of large droplets from the upper respiratory tract, where we now know the coronavirus lives and replicates. Large droplets, caused by talking, sneezing, coughing, and even singing, quickly succumb to gravity and land on surfaces or other people. Any face covering helps prevent these larger droplets from entering the external environment and infecting others. It’s really that simple.
It is true that the coronavirus can spread through aerosol, or very small particle transmissions that are expelled through the lower respiratory tract. These small particles may exist in the air for hours at a time, and a cloth facemask is unlikely to filter all of these nanoparticles. The risk of aerosol transmission is higher in healthcare settings, particularly by intubating a patient or by spending prolonged time in close contact with a symptomatic patient. This is why healthcare providers need to wear respirator masks, which are better equipped to filter out these particles than cloth masks. But aerosol transmission is less likely to occur outside of these settings, particularly from an asymptomatic or presymptomatic carrier.
Despite all of the promising scientific evidence that supports the use of masks in reducing the spread of the coronavirus, an important variable remains: the protection is imperfect. It is a way to reduce transmission, but it won’t completely eliminate it. Still, wearing a mask is a crucial component in flattening the curve. It’s easy to do, and we need to use all of the tools available to fight the pandemic.
The coronavirus has an Achilles heel – It cannot live without you. The virus needs a host to survive. When it can’t find a new host, it dies. Wearing a mask helps break the chain of transmission, and right now, that is our best and only defense.
Bottom line: Masks decrease coronavirus transmission, mostly by preventing spread to other people.
Myth 2: Masks decrease oxygen intake, which results in cognitive decline and other dangerous health issues.
Cloth masks, and even surgical masks, do not fit tightly and therefore pose a very low risk of hypoxia (low oxygen) or hypercapnia (too much carbon dioxide). We actually have decades of evidence on this and millions of data points: Doctors and nurses, who perform hours long surgeries while donning surgical masks, do so on a daily basis without long term effects such as cognitive decline. Many doctors and nurses work in these conditions well into their sixties and seventies (and beyond!), without breathing issues and they remain as sharp as ever. Short term effects, such as shortness of breath, are rare, mild, and easily reversible by removing the mask.
Respirators, such as N95 masks, should be reserved for certain medical personnel and are not recommended for the general public, have a much tighter fit, and therefore pose a slightly higher risk of decreased oxygen intake. A 2016 study from Johns Hopkins demonstrated that while respirators do succeed in providing necessary protection to healthcare providers in specialized settings, it is possible that prolonged use can compromise performance and reduce efficiency. Still, these side effects of reduced oxygen intake occur acutely and coincide with physical symptoms that the user can easily and immediately recognize. Taking off the mask to increase oxygen intake when this occurs solves the problem quickly. There is zero scientific evidence that wearing masks, respirators or otherwise, cause silent, degenerative effects, such as cognitive decline.
But remember: the general public is directed to wear cloth masks, not respirators, so the risk of these complications remains incredibly low. Moreover, the recommendation to wear masks applies to public spaces where social distancing is difficult, such as in grocery stores, retail settings, and on public transportation. An hour-long session with a cloth mask is certainly less likely to induce hypoxia than wearing a respirator for a prolonged amount of time. That being said, those with certain medical conditions, such as severe breathing issues or those who cannot independently remove their own masks, may be at higher risk of developing side-effects and can appropriately opt out of wearing a mask. But even in these cases, many experts suggest solutions to ensure safety while masking up. Lastly, children under 2 years of age should not wear a mask.
Bottom line: Wearing a cloth mask poses very little risk of hypoxia and no risk of long-term cognitive decline. If you feel short of breath, lightheaded, or dizzy while wearing a mask, simply take it off to quickly recover. Those with certain medical conditions and children under 2 should not wear masks.
Myth 3: Masks cause rashes and other skin diseases
Wearing a mask repeatedly or for a prolonged period of time can potentially cause a number of unpleasant symptoms, including rashes, skin breakdown, breakouts, and more. Ensuring that your cloth mask fits well and is clean, breathable, and made of moisture wicking fabric will reduce your chances of developing any of these issues. The technology in our Hemp Black fusion / FACE MASK can help.
Bottom line: Masks can cause some skin issues, but they pose a far less serious threat than the coronavirus. Solutions exist, so ensure you are selecting the best mask.
Myth 4: Masks actually increase chances of contracting Covid-19
We have heard some erroneous claims that wearing mask causes one to “reinhale” viral particles and thus increase the infection. This is not how virology works and has no scientific credibility. Once you are infected with the virus, it replicates in your cells independently. While someone may exhale viral particles, known as shedding, this does not affect the same individual’s infection.
There is at least some merit, however, to the concern about masks promoting one’s risk factor: Touching the face increases chances of infection. If you touch a contaminated surface and pick up viral particles on your hand, then touch your face with that hand, you can introduce the viral particles to mucous membranes in your nose, eyes, and/or mouth where it replicates, causing infection. Without masks, studies show that we touch our faces 16 to 23 times every hour. With masks, it’s reasonable to assume that number could increase. It is an exercise in self-discipline to decrease or eliminate this habit. This is why we all need to be diligent about washing our hands, so that we do not transmit viral particles from our hands to other areas of the body vulnerable to infection. We also need to be conscientious about touching our face, with or without a mask on.
The good news is that we have learned that the coronavirus spreads primarily from person to person, and less so through surfaces. While contaminated surfaces are not the primary driver of Covid-19 infections, the risk still exists. But not all surfaces or materials present equal risk. For example, a recent study in the New England Journal of Medicine showed that the new coronavirus can live on stainless steel and plastic for up to 72 hours and on cardboard for up to 24 hours. While the virus was still detected on surfaces at these prolonged time points, it had significantly deteriorated. Copper, however, kills viral particles on contact. The same study measured zero viral particles on copper after 4 hours. A scientifically evaluated copper mask, then, significantly decreases risk of contamination.
Bottom line: Wash your hands, stop touching your face, and use a washable copper mask.
Myth 5: The CDC changed their opinion on mask recommendation, so none of this makes sense.
It is true that the CDC initially recommended against masks for the general public. They changed that recommendation because more scientific evidence emerged to support the benefits of masks during the coronavirus pandemic. This has always been true of science and medicine; When new and compelling research materializes, we shift our practices accordingly.
Additionally, the U.S. experienced a shortage of critical PPE (personal protection equipment), including masks, for those with the highest risk of infection: healthcare workers on the frontlines of the crisis, who risk continued exposure while treating patients. It is still critical to reserve respirators, such as N95 masks, for medical personnel while they are on duty in these high-risk settings. Cloth masks, however, are recommended for the general public.
Bottom line: The CDC now recommends cloth masks because science said so.
Myth 6: Masks decrease human connection.
We cannot think of a better way to be a good human than to potentially and quite literally save lives. Because many of those with coronavirus are asymptomatic, those who feel perfectly healthy can unknowingly infect others. Masks reduce this risk, as explained above. While many coronavirus cases are mild, some are deadly. We do not fully understand who is most vulnerable to severe infections, and unexpected variables, such as blood type, continue to emerge as risk factors for severe infection. We must consider others and do our best to protect everyone. Human connection is impossible if we don’t have others around. Wearing a mask is an exercise in altruism.
Bottom line: Save lives and smile with your eyes.
Myth 7: Masks are the solution to solving the coronavirus pandemic.
As discussed above, scientific evidence endorses masks as a way to decrease coronavirus spread. But wearing a mask alone is not a complete solution. Instead, it is part of a comprehensive strategy that includes diligent hand washing, social distancing, increasing sanitization measures, decreasing touching your face, isolating when sick, and getting a Covid-19 test when appropriate. Wearing a mask does not replace these other practices that are vital in reducing infections.
Bottom line: Continue to follow all infection control guidance, including wearing a mask in public.
Written by Dr. Alex Capano, DNP, CRNP, FNP-BC, Chief Science Officer at Ecofibre